Activity
- Refer to your surgeon-specific patient education and hospital discharge instructions.
- Perform your prescribed exercises 2-3 times each day.
- Avoid spending long periods of time seated or in bed.
- Assume a routine that has you moving with your walker every 1-2 hours to avoid stiffness.
- Take a walk 3-4 times a day, gradually increasing the distance.
- Use your walker at all times, until advised otherwise by your surgeon or therapist.
- Progress to use of cane as directed by your therapist or physician.
- For knee replacements, it is very important to regularly bend and straighten your knee fully to work on regaining functional knee range of motion. Avoid placing pillows directly under your knee. Avoid keeping your knee in one position for prolonged periods.
- For hip replacements, use the recommended adaptive equipment to complete self-care tasks until your surgeon discontinues your hip precautions.
- Limit stair climbing if advised by your surgeon.
- You may ride in a car. If traveling long distances, be sure to stop frequently and walk.
- Your physician will recommend to you when you are cleared to drive a vehicle
- For swelling of the lower legs, elevate your leg while in bed. Elevate the leg on 2-3 pillows turned lengthwise under your leg for 40 minutes, 2-3 times a day, “toes above your heart.”
- You may bear weight on your surgical leg as tolerated, unless instructed otherwise by your surgeon.
- The goal is to gradually resume your normal daily routine.
Whether you have reached all your goals within three months or not, it is highly recommended you continue to participate in an exercise program. Exercise can help maintain healthy muscles around your new joint. With permission from your surgeon and primary care doctor, it is recommended you exercise 3-4 times per week with each session lasting 20-30 minutes. Low-impact activities are recommended; these include walking, riding a bike, participating in an exercise class, or performing a home exercise program.
Incision Care
- Remove the waterproof dressing in 1-2 weeks, per your surgeon’s directions. You are permitted to shower with this dressing on.
- After the dressing has been removed, gently clean the entire length of the incision with soap and water daily. Pat dry.
- Do not apply lotions, creams or powders on the incision until you follow up with your surgeon.
- You may shower. No baths. Do not submerge your incision.
Preventing Blood Clots
- Use blood thinning medications as directed by your surgeon.
- Wear your support hose during the day for 2-3 weeks. You may need assistance to apply.
- Perform your exercises faithfully.
Pain Control
- Make a schedule to take your pain medicine regularly if needed. Be sure to take pain medicine at least 30 minutes before physical therapy and planned exercises.
- Time your pain medicine so you take a dose before you go to bed. This will help keep you comfortable through the night while you sleep. If you wake up in the middle of the night, you may need to repeat the dose.
- You can start taking pain medicine less often as your pain improves. Gradually, you will wean yourself off the prescription pain medicine and take Tylenol (acetaminophen) instead.
- If you should need pain medication refills, you should call your surgeon’s office during office hours. Look ahead so that you don’t run out over the weekend.
- Try to change your position at least once every hour while you are awake.
Why use ice?
The use of ice can relieve pain, swelling, inflammation or spasm in your new joint. Cold causes the blood vessels to constrict, which reduces blood flow. After removing the ice, the body’s natural response is for the blood vessels to dilate, which in turn brings new blood to the surgical site to facilitate healing. This cycle also creates a pumping action which removes swelling, allowing your new joint to move more easily. Additionally, icing decreases activity of the nerve fibers which reduces pain. It is important that you are consistent with your icing program after surgery as regular icing assists with the management of post-operative swelling and pain, when pain and swelling are effectively managed it allows you to steadily progress your activity level.
Early in your recovery it is recommended that you ice the surgical area at least 4-5 times a day for 15-20 minutes each icing session. An effective schedule is to ice in the morning, at noon, mid-afternoon, evening and before bed. Do not use ice while sleeping. When icing always place a towel or pillowcase between the ice and your skin as direct contact with ice can cause damage to the skin. It is also important to monitor your skin when using ice; the skin should be pink, if the skin appears white, remove the ice until the pink flush is regained. If this occurs you may need to use an additional layer of protection between the ice and your skin. When icing multiple times per day, it is important to allow the tissue to rewarm for at least 45 minutes to an hour between icing sessions.
As you progress through the rehabilitation process you can begin intermittently icing as needed for symptom control. It is also recommended to ice following physical therapy appointments, after completing your individualized exercise program, or after any prolonged standing or walking.
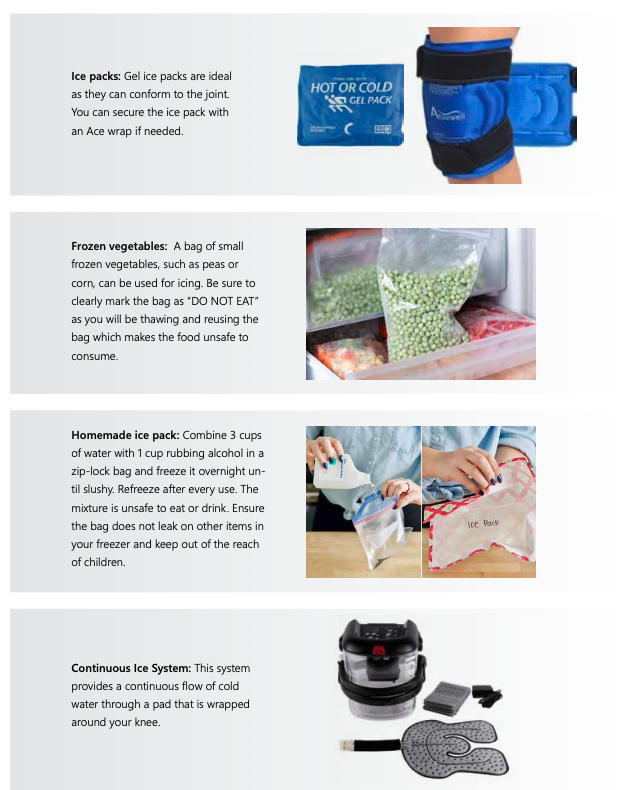
Any of the below options can be used to effectively ice your new joint:
Managing Leg Swelling
Leg swelling is a common occurrence following joint replacement surgery. Excessive swelling may interfere with your return to normal activity and could lead to more serious complications. Leg swelling occurs most frequently after a patient leaves the hospital. When you spend an extended period time in a seated position, swelling occurs. This is because blood is returned to the heart through the venous system. Proper blood return from the legs depends on the integrity of the valves within the veins and is assisted by muscle contraction during activity. Valves allow blood to move toward the heart and keep gravity from making blood flow back down the leg. Following joint replacement surgery, muscle contracture is decreased because of low activity level.
The veins become distended and the valves become less effective. You can help minimize the swelling by changing your body’s position, so that gravity can work in your favor. The position changes must involve a complete horizontal lying down with the legs elevated higher than the level of the heart. In this position, excess fluid is drained from the leg by force of gravity.
The position is easily accomplished by lying on a sofa or bed, putting a pillow under the involved knee and calf and raising the leg high above the level of your heart. Place 1-2 pillows lengthwise under your leg or simply under your ankle.
Drainage by gravity cannot occur if you are sitting in a chair with your leg elevated on a stool. Remember, the leg must be higher than the level of your heart.
Another way to help improve swelling is to walk, so that the muscles contract and act as a pump to send the fluid back to the heart. Ankle pump exercises are also helpful for contracting muscles and reducing swelling. While lying in bed, point and flex both feet slowly.
Lastly, swelling can be controlled by wearing compression stockings. These stockings should be knee or thigh length and worn during the day. Put them on in the morning and remove them at night. Wear them for 2-3 weeks. Hand wash the stockings and hang them up to dry.
Staying Healthy
- Eat a well-balanced diet.
- Maintain a healthy weight.
- Exercise. Remember, in the first few weeks it is very important to follow your therapist prescribed home exercise program.
- Continue to avoid tobacco products as they hinder the healing process.
- Utilize your incentive spirometer during any extended periods of rest.
- Stop and think...use good judgment.
General Guidelines
- After hip replacement surgery avoid sitting in a chair where you are positioned with your hips higher than your knees as this places stress on your new hip joint.
- Avoid sitting or lying on low and soft surfaces.
- Keep frequently used objects positioned between hip and shoulder level.
- Use a reacher for objects on the floor.
- Keep walkways at home clear and well lit.
- Always wear rubber-soled, closed-heeled shoes or slippers.
Constipation
Taking pain medicine and decreased activity can increase the risk of constipation. Use stool softeners as recommended by your physician or pharmacist, usually two times a day. Be sure to eat plenty of fruits and vegetables; this will help normalize your bowel movements. Also, drink 6-8 glasses of water each day. You may need to take a laxative periodically.
Returning to Work
You may not return to work 6-12 weeks after the operation. Some patients do return earlier, depending on the nature of their work, how flexible their workplace is with returning on a part-time basis initially, or whether work is done from home. We generally tell employers 6-12 weeks, but you may return sooner if you are physically ready. It is easier to return to work sooner than to request more time off. Discuss this with your surgeon if you have additional questions.
